
When Kavitha (name changed) first came to see me three years ago, she was not seeking help for anxiety or depression in the traditional sense. She had recently been diagnosed with Type 2 diabetes and rheumatoid arthritis, and she sat in my office with tears streaming down her face, saying words I have heard from hundreds of clients since: "I feel like I have lost myself."
In my fifteen years of practicing psychology in Hyderabad, I have witnessed how chronic illness does far more than affect the body. It reshapes identity, transforms relationships, alters life plans, and profoundly impacts mental health. Yet this psychological dimension of chronic illness is often overlooked in our healthcare system, where the focus remains primarily on managing physical symptoms.
Today, I want to address something that affects millions of Indians but is rarely discussed openly: the mental health challenges that accompany living with a chronic condition, and more importantly, how you can protect and nurture your psychological wellbeing through this journey.
The Hidden Burden: Understanding the Emotional Impact
According to recent studies, individuals with chronic illnesses are two to three times more likely to experience depression and anxiety compared to the general population. In India, where an estimated 116 million people live with diabetes alone, and countless others manage conditions like heart disease, chronic kidney disease, autoimmune disorders, and cancer, this represents a massive mental health challenge that often goes unaddressed.
But statistics only tell part of the story. In my practice, I have learned that the emotional impact of chronic illness is deeply personal and multifaceted.
Loss of Identity: Many of my clients describe feeling like strangers in their own bodies. Venkat (name changed), a former marathon runner diagnosed with multiple sclerosis at 42, told me, "I used to be the guy who ran 10 kilometers before breakfast. Now I am the guy who needs help getting out of bed some mornings. I do not recognize myself anymore."
Unpredictability and Anxiety: Chronic illness often brings profound uncertainty. Will today be a good day or a bad day? Will this treatment work? What will my life look like in five years? This constant uncertainty can generate persistent anxiety that exhausts the mind as much as the illness exhausts the body.
Social Isolation: Cancelled plans, friends who do not understand, the inability to participate in activities you once enjoyed—chronic illness can shrink your world dramatically. Many of my clients describe feeling increasingly isolated, even within their own families.
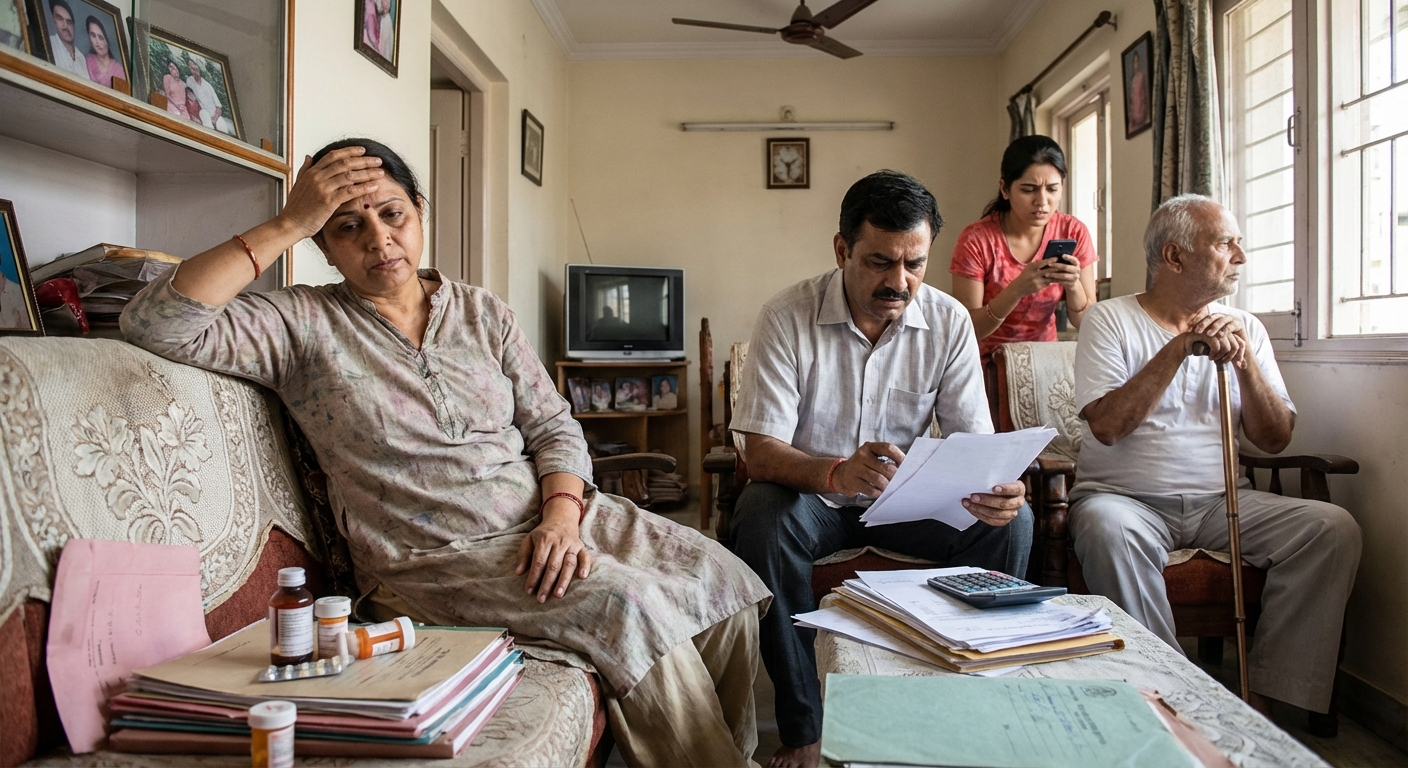
Financial Stress: The cost of managing a chronic condition in India—medications, specialist consultations, tests, dietary requirements—can create enormous financial pressure, which in turn affects mental health.
Relationship Strain: Chronic illness does not happen in isolation. It affects marriages, parent-child relationships, friendships, and professional connections. The person who is ill often struggles with guilt about being a burden, while family members may experience caregiver fatigue and their own grief.
The Grief You Are Allowed to Feel
One of the most important things I tell my clients is this: what you are experiencing is grief, and it is entirely valid.
When you receive a chronic illness diagnosis, you are not just learning about a medical condition. You are saying goodbye to the life you expected to have, the body you thought you could count on, the future you had planned. This is a profound loss, and it deserves to be mourned.
In my experience, people with chronic illness often move through stages similar to the grief process Elisabeth Kubler-Ross described:
Denial: "This cannot be happening to me. The tests must be wrong. If I just ignore it, maybe it will go away." I have had clients who refused to take medications or acknowledge their diagnosis for months, hoping it would simply disappear.
Anger: "Why me? What did I do to deserve this? It is not fair." This anger might be directed at doctors, at God, at family members, or at oneself. Meera (name changed), diagnosed with lupus at 28, spent months furious at the universe. "I did everything right," she told me. "I ate well, exercised, never smoked. And this is what I get?"
Bargaining: "If I follow the diet perfectly, maybe I can reverse this. If I pray hard enough, maybe I will be healed." While hope and proactive management are healthy, bargaining sometimes reflects a difficulty accepting the permanence of the condition.
Depression: Deep sadness about what has been lost and what the future now holds. This is often when people come to see me—when the reality of living with chronic illness truly sinks in.
Acceptance: This does not mean being happy about being ill. It means acknowledging reality and finding ways to live meaningfully within your new circumstances. Acceptance is not a destination but a process that often needs to be revisited.
What I want you to understand is that these stages are not linear. You may cycle through them repeatedly, especially when your condition changes or during difficult periods. This is normal. Give yourself permission to grieve, again and again if necessary.
Practical Strategies for Protecting Your Mental Health

After years of working with individuals living with chronic conditions, I have identified strategies that consistently help protect and improve mental wellbeing. Here is what I recommend:
1. Build a Relationship with Your Illness
This may sound strange, but hear me out. Fighting against your illness constantly—denying it, resenting it, treating it as an enemy to be conquered—is exhausting and often counterproductive.
Instead, I encourage clients to develop a kind of working relationship with their condition. This means learning about it thoroughly, understanding its patterns in your specific body, and finding ways to accommodate it without letting it dominate every aspect of your life.
Suresh (name changed), who has lived with Crohn's disease for over a decade, described it beautifully: "I finally stopped trying to defeat my illness and started learning to live alongside it. It is like having a difficult housemate—we have had to establish boundaries and routines that work for both of us."
2. Redefine What a Good Day Looks Like
Chronic illness often means letting go of previous standards and definitions of success. A good day might no longer mean completing a 12-hour workday. It might mean managing your symptoms well, spending quality time with family, or simply getting through your daily routine without a flare-up.
I work with clients to identify what is genuinely important to them and to measure their days against those values rather than against their pre-illness capabilities or others' expectations.
3. Pace Yourself and Protect Your Energy
Many chronic conditions involve fluctuating energy levels. I teach my clients the concept of "energy budgeting"—treating your daily energy like a limited resource that must be allocated thoughtfully.
This means learning to prioritize, to say no without guilt, to rest before you are completely depleted, and to plan important activities for times when you typically have more energy. It also means letting go of the guilt that often accompanies rest.
4. Maintain Social Connections, Even When Difficult
Isolation is one of the greatest risks to mental health during chronic illness. I encourage clients to:
- Be honest with a few trusted people about what they are experiencing
- Find ways to socialize that accommodate their limitations (phone calls if outings are difficult, brief visits rather than lengthy gatherings)
- Connect with others who understand—whether through support groups, online communities, or simply one other person living with a similar condition
- Accept help when offered, even when it feels uncomfortable
5. Practice Mindfulness and Present-Moment Awareness
When you have a chronic illness, it is easy to spend all your mental energy worrying about the future or mourning the past. Mindfulness practices help anchor you in the present moment, where life is actually being lived.
This does not mean ignoring your feelings or pretending everything is fine. It means developing the ability to observe your thoughts and emotions without being completely overwhelmed by them. Even five minutes of daily mindfulness practice can make a meaningful difference.
6. Address Negative Thought Patterns
Chronic illness often generates particular thought patterns that worsen mental health:
- Catastrophizing: "This symptom means everything is getting worse."
- All-or-nothing thinking: "If I cannot do things the way I used to, there is no point doing them at all."
- Guilt and self-blame: "If only I had taken better care of myself, this would not have happened."
- Comparison: "Everyone else seems to be living normal lives while I am stuck dealing with this."
7. Maintain Elements of Your Pre-Illness Identity
While chronic illness inevitably changes you, it does not have to erase who you were before. I encourage clients to find modified ways to engage in activities they loved, to maintain roles and relationships that give them meaning, and to continue pursuing interests and goals where possible.
Lakshmi (name changed), an artist diagnosed with severe fibromyalgia, thought she would never paint again. Together, we explored adaptations—shorter sessions, ergonomic tools, different media—that allowed her to continue creating. "Painting is not what it was before," she told me, "but it is still mine. It still feeds my soul."
Building Your Support System

No one should navigate chronic illness alone. Building a robust support system is essential for mental health. Here is what an effective support system might include:
Medical Team: Beyond just treating your physical symptoms, your healthcare providers should be partners in your overall wellbeing. Do not hesitate to discuss mental health concerns with your doctors—or to seek new providers if you feel unheard.
Mental Health Professional: A psychologist or counselor experienced with chronic illness can provide invaluable support. Therapy offers a space to process difficult emotions, develop coping strategies, and work through the challenges specific to your situation.
Family and Friends: Educate those closest to you about your condition and your needs. Be specific about how they can help—and equally specific about what is not helpful. Not everyone will respond perfectly, but most people want to support you if they understand how.
Peer Support: Connecting with others who truly understand what you are going through—because they are living it too—can be profoundly comforting. Look for support groups, either in person or online, for your specific condition or for chronic illness in general.
Practical Support: Sometimes you need help with groceries, transportation to appointments, or household tasks. Identifying resources for practical support reduces stress and preserves your energy for healing.
Supporting a Loved One with Chronic Illness
If someone you love is living with a chronic condition, your role is crucial. Here is my guidance:
Listen More Than You Advise: Resist the urge to immediately suggest solutions or treatments you have read about. Often, your loved one simply needs to be heard and validated.
Learn About Their Condition: Education helps you understand what they are experiencing and anticipate their needs.
Ask How You Can Help: Rather than assuming, ask specific questions. "Would you like company at your next appointment?" "Can I bring dinner on Thursday?"
Be Patient with Fluctuations: Chronic illness is unpredictable. Plans may need to change. Your loved one may seem fine one day and struggle the next. This is the nature of chronic conditions.
Take Care of Yourself: Caregiver burnout is real. You cannot pour from an empty cup. Ensure you are attending to your own physical and mental health, and seek support if you need it.
When to Seek Professional Help
While some degree of emotional difficulty is normal when living with chronic illness, certain signs indicate that professional mental health support is needed:
- Persistent feelings of hopelessness or worthlessness
- Loss of interest in activities, relationships, or life in general
- Significant changes in sleep or appetite
- Difficulty functioning in daily life beyond what your physical condition requires
- Thoughts of self-harm or suicide
- Using alcohol or substances to cope
- Severe anxiety that interferes with medical treatment or daily activities
A Message of Hope

I want to end with something important: living with chronic illness is hard. It is okay to acknowledge that. You do not need to be inspiring or brave or positive all the time. You are allowed to have difficult days, to grieve, to feel angry or sad or scared.
But I also want you to know that it is possible to live a meaningful, fulfilling life while managing a chronic condition. I have seen it countless times. Not a life without challenges—but a life with purpose, connection, joy, and hope.
Kavitha, whom I mentioned at the beginning, came to see me convinced that her life was essentially over at 45. Three years later, she manages her conditions alongside a rich life—a renewed marriage, a part-time career she loves, and a sense of peace she says she never had even before her diagnoses.
"I am not grateful for being ill," she told me recently. "But I am grateful for who I have become through learning to live with it. I am stronger than I knew. And life is more precious than I ever realized."
This can be your story too. Chronic illness may be part of your life, but it does not have to define your life. With proper support—medical, psychological, and social—you can protect your mental health and thrive.
---If you are in Hyderabad and struggling with the mental health challenges of chronic illness, I invite you to reach out. At my practice, I offer specialized support for individuals navigating life with chronic conditions, helping them process grief, develop coping strategies, and find their path to psychological wellbeing. I provide both in-person consultations at my Hyderabad clinic and online sessions for those who prefer or require the convenience of virtual care.
Remember: taking care of your mental health is not a luxury—it is an essential part of living well with chronic illness.
---Sudheer Sandra is a licensed psychologist and career counselor based in Hyderabad, India, with over 15 years of clinical experience. He specializes in anxiety, depression, relationship issues, and career counseling. Sudheer is committed to providing compassionate, culturally sensitive mental health care and believes that psychological wellbeing is fundamental to overall health, especially for those managing chronic conditions.
